Dementia needs you

Dementia is a health condition that affects the entire person. It changes cognitive abilities, functional capacity, behaviour, interpersonal relationships, and physical wellbeing. Through your knowledge and skills as a healthcare professional you can provide significant benefits to people with dementia and their carers and make important contributions to their quality of life. Using the present programme will help you improve your knowledge and skills about dementia and will make your professional life easier, more effective, and more rewarding.
Dementia is a global health problem
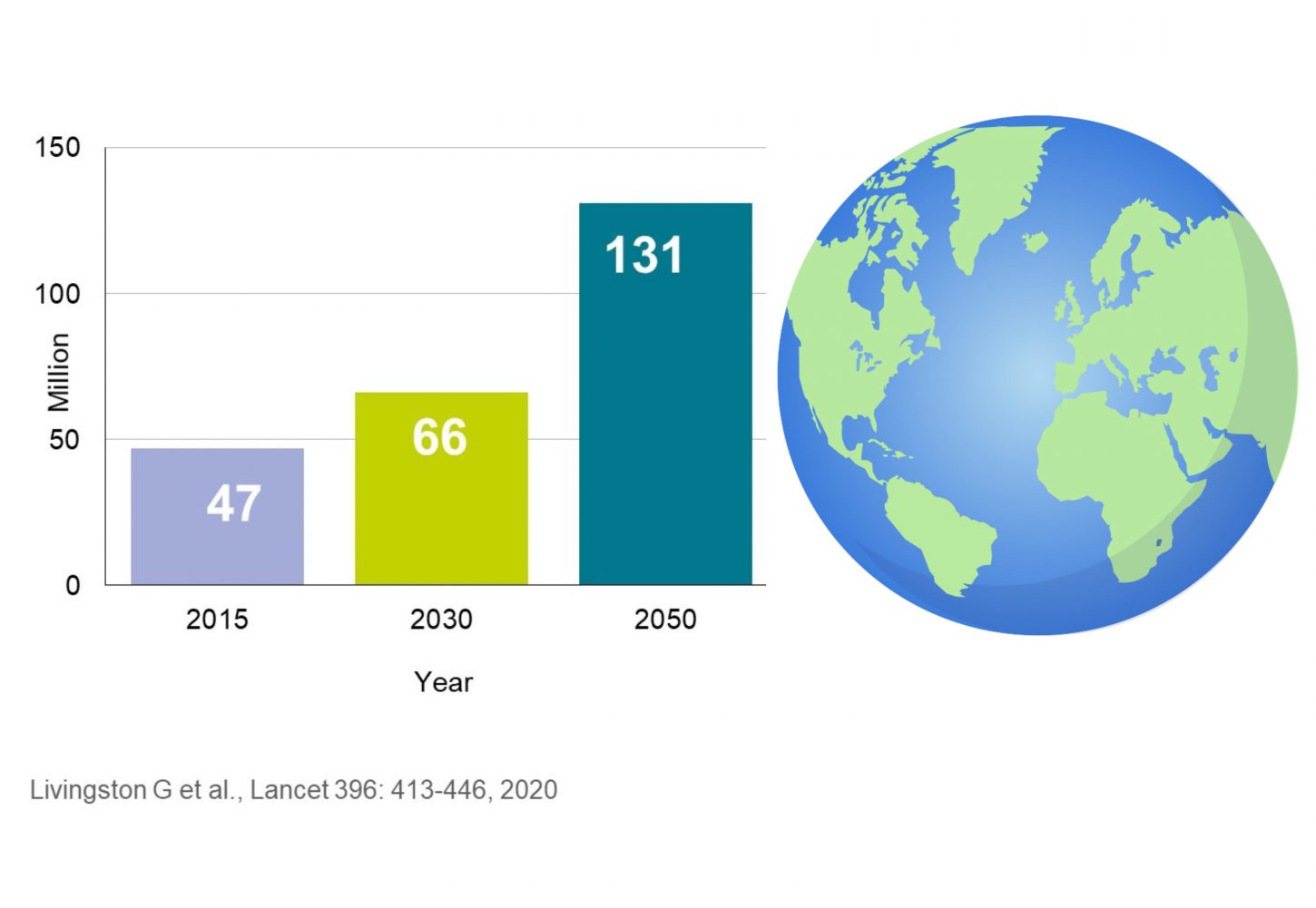
Dementia is a rapidly growing societal and public health challenge, and it is almost impossible to find someone, who has not been in touch with dementia, at least through friends or family. Worldwide, approximately 47 million people were living with dementia in 2015. Due to the increase in life expectancy this number is expected to increase to 66 million by 2030 and to 131 million in 2050.
Number of people living with dementia worldwide
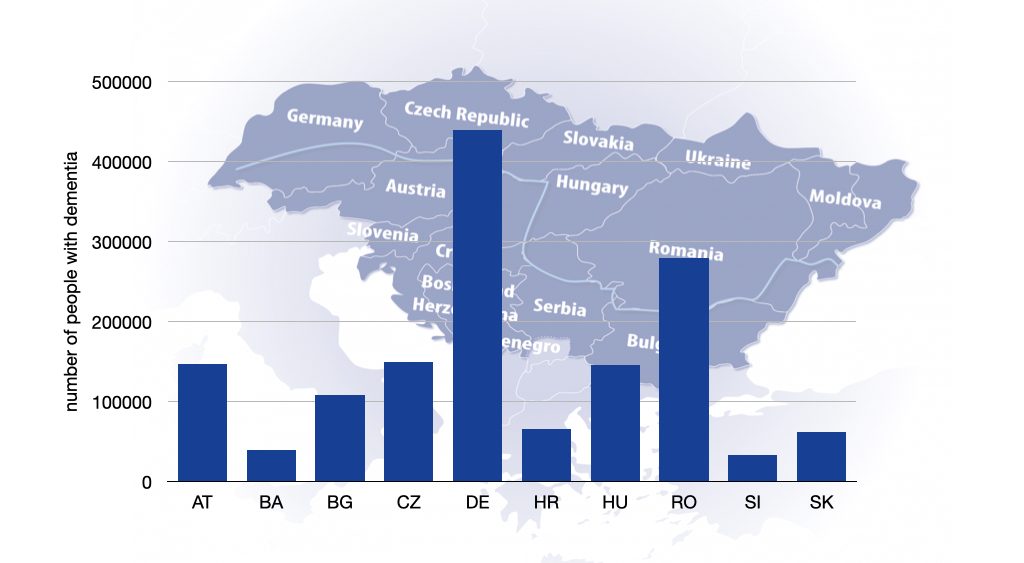
How many people are living with dementia in Danubian countries ?
Dementia is a major health and social challenge in the Danube region. At least 1.6 million older adults are currently living with dementia in this part of Europe.
Number of people living with dementia in the Danube region
Dementia forecasts and healthcare systems
The rising number of people with dementia will lead to an increase of people requiring long-term care by 30 % while the number of individuals who can provide long-term care will decline. An additional problem in the Danube Region is the outward migration of skilled health workers („care drain“) which is driven by economic and health-related reasons and has resulted in a lack of qualified health personnel and reduced family support in the “sending” countries.
However, the challenge of dementia is not always reflected in national policies, and important steps for dealing with the challenge are not undertaken. In view of the growing burden of dementia, the dramatic impact the condition has on people’s lives and the diminishing resources for coping with it, improvement and sustainability of dementia care has to be placed high on political agendas in the Danube Region. In particular, access to dementia-related knowledge and skills among health and social professionals is key to ensure high-quality care to this vulnerable population.
Dementia is a pattern of symptoms that can have many causes
Dementia is not a disease but a pattern of symptoms (the medical term is „syndrome“) that can be the result of many causes, including diseases of the brain where nerve cells are gradually lost (neurodegenerations), infections, inflammations, head trauma, tumours and others. The symptoms of dementia refer to cognitive ability, performance on activities of daily living, behaviour, emotional state and social conduct, and physical functioning. The pattern of symptoms shows a broad variation, depending on which parts of the brain are most severely affected by the underlying cause.
Dementia has a profound impact on the person and the family
Dementia has a huge impact on the entire person in terms of personal identity and self-esteem. It also changes the roles and relationships within the family and in wider social networks. The gradually evolving symptoms ultimately lead to increasing disability.
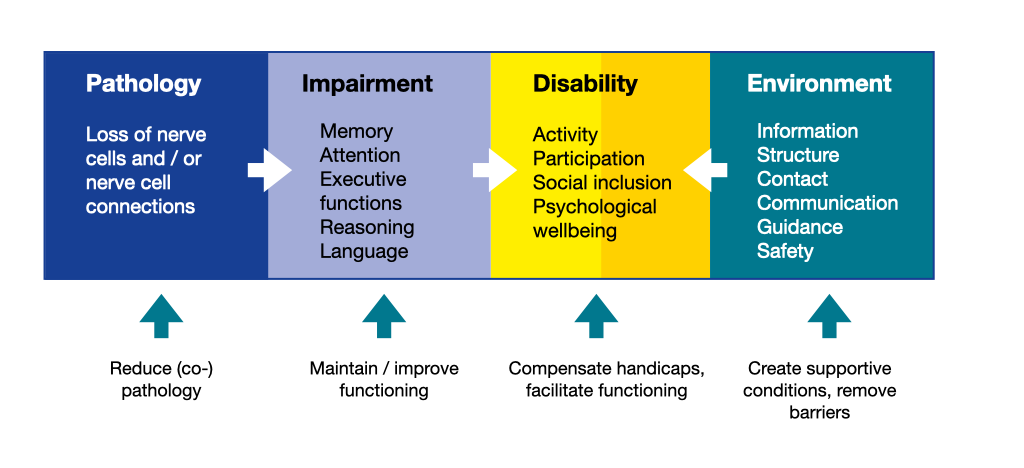
WHO’s International Classification of Functioning, Disability, and Health
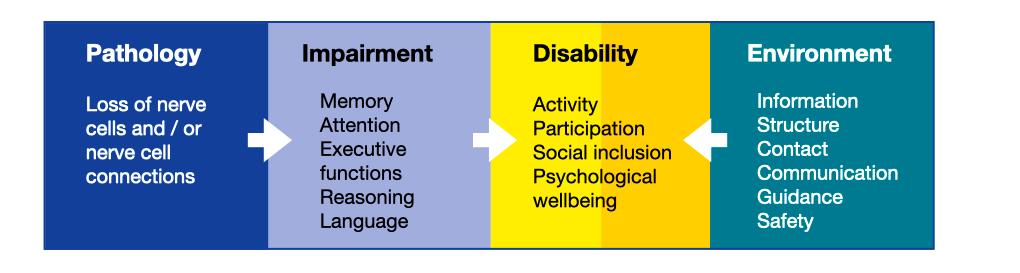
Therefore, dementia has a profound effect on the individual’s quality of life. However, the quality of life in people with dementia is not determined solely by the cognitive impairment that results from the pathological process. At the early stage, it depends to a great extent on autonomy, continuation of individual lifestyle, attainment of personally important goals, meaningful activities and participation in life; at the moderate stage on safety, appreciation and social connectedness; and at the severe stage on comfort, dignity and emphatic relationships. Thus, factors in the environment can be supportive and act in a compensatory way. Importantly, these factors are potentially modifiable.
Many professions can contribute to improving the quality of life of people with dementia and their carers
The quality of life of people with dementia can be improved
Dementia has long been considered as a condition that can neither be prevented nor treated. However, recently there has been a switch towards a more optimistic perspective. Although there is still no cure for most diseases underlying dementia, many of its signs are known to be manageable, and the quality of life of people with dementia and their family carers can be improved.
The primary objectives of dementia management are providing an optimal quality of life throughout the course of the illness by maximising functional ability and promoting independence, regaining lost function when there is a potential to do so, and adapting to lost function that cannot be regained. The figure below illustrates that interventions can apply on many levels.
The life of people with dementia can be full of respect, dignity, and support. Successful collaboration of all actors involved in management of dementia, including occupational therapists, social workers, nurses, physiotherapists, general practitioners, psychiatrists, neurologists, or psychologists, is essential for maintaining the quality of life of people with dementia and their families.
Examples
Jane struggled with managing the everyday care for herself and the household, she was unsure about whether she took her pills, whether she picked out the mail or how to use the new washing machine. A social worker recommended her assistive technologies with reminders and notes which helped her to better organise her day.
Diana observed problems with word finding in her husband. Based on an advice from occupational therapist she found materials for cognitive training at the memory clinic and engaged with him in sessions of training when having conversations on different topics.
Daniel felt anxious and nervous during the day and he was not sure about the reason. Sessions of playing piano together with a volunteer helped him to calm down and feel more peaceful, even without medication.
