What are major needs of people with dementia?
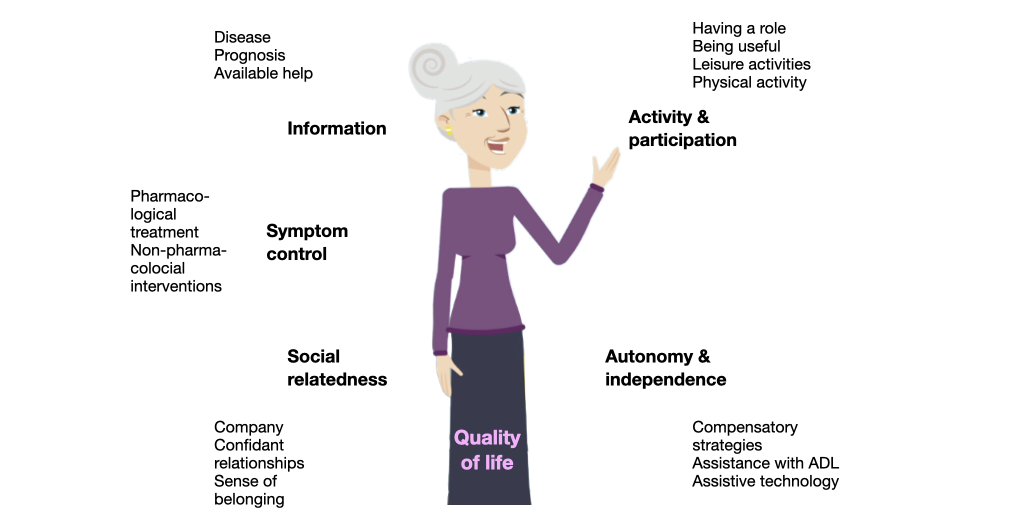
The needs of people with dementia are complex and individually diverse. They can be assigned to five major categories: information, symptom control, activity and participation, social relatedness, autonomy and independence. Interventions that meet the needs contribute to improving their quality of life. The needs of people with dementia change as the condition progresses.
Five categories of needs
Meeting needs improves quality of life
Changing of needs during the course of dementia
| Stage | Information | Treatment & care | Psychosocial needs | Physical needs |
|---|---|---|---|---|
| Early | Disease Prognosis Available services Financial support Advance directives | Antidementia drugs Non-pharmacological interventions Assistive technology Comorbidities | Activity Participation Being useful Having a role | Exercise |
| Middle | Available services Help with transitions | Memory aids ADL assistance Behaviour management Mobility Self-care Safety Assistive technology | Activities Emotional support Social contact Relationships Acceptance Preservation of identity Spiritual support | Basic nursing Nutrition Exercise |
| Late | Physical wellbeing Pain management | Comfort Safety Company | Basic nursing Hygiene Nutrition Sleep |
Meeting the needs improves quality of life
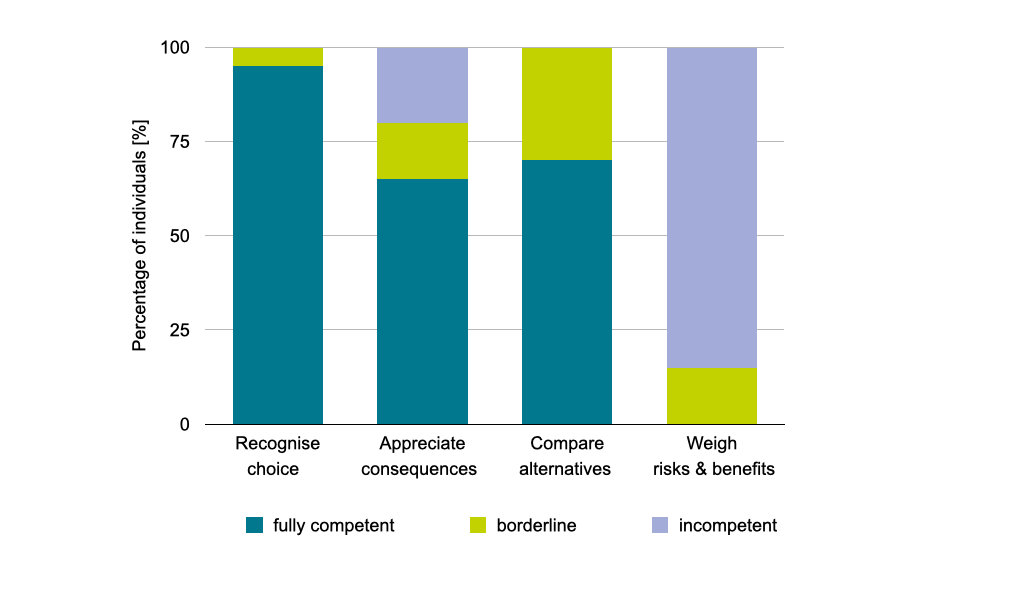
Can people with dementia participate in decision-making?
The ability to evidence a choice and making the reasonable choice is unimpaired at the stage of mild dementia. However, complex appreciation, reasoning and understanding are already compromised. The ability to provide complex consent rapidly declines over time. This shows that people with dementia need to be involved in decision-making at an early stage. Moreover, decisions and choices must be presented in a simple, understandable way and step-by-step.
Decision-making capacity of people with mild dementia
What are the major needs of informal carers?
The major needs of (family) carers of people with dementia include information (about diagnosis, prognosis, treatment options and available services, organising and financing care), strategies for dealing with problem behaviours of the person with dementia (apathy, aggressiveness, irritability and others), ways of coping with own difficult emotions (anger, distress, loneliness, grief, depression), advice for managing the change in roles and relationships (novel tasks, role conflict, loss of mutuality and closeness) and coaching on communication.
Needs of informal (family) carers
| Stage | Information | Psychosocial needs | Services |
|---|---|---|---|
| Early | Receiving a diagnosis Symptoms and progression Dealing with memory loss Access to services Meaningful activities | Accepting the diagnosis Dealing with changing roles and relationship | Carer support group Assistance with housekeeping Home helpers Assistive technology |
| Middle | Managing behavioural problems (agitation, irritability, apathy) Dealing with physical symptoms (nutrition, hygiene, incontinence) | Dealing with own emotional problems (guilt, anger, grief) Role conflict Pursuing own interests Fighting isolation | Own health problems Financing care Safety issues Environmental modification Respite care Adult day care |
| Late | Nursing home admission Choosing appropriate institution End-of-life care | End-of-life decisions | Accessible and affordable facilities |
Meeting complex needs requires a care plan
Needs do not arise all at one time, and they change considerably during the course of dementia. Interventions need to be planned and coordinated in order to come at the point of need and take advantage of synergies. Ideally, the professionals involved should work together to create an individual care plan that takes into consideration individual needs related to gender, ethnicity, age, level of education, previous lifestyle and physical health. The care team should be led by a physician (e.g. the GP), nurse or social worker.
Meeting complex needs requires a team and a plan
Collaboration pays
Working as a team requires some extra efforts and time of professionals, but it is likely to pay in terms of greater treatment efficacy, less requirement of repeat visits and crisis management, and greater treatment satisfaction on the part of people with dementia and carers. Working together provides benefits for everyone involved.
